Can Packaging Optimize Hospital Hygiene & Handling?
This 2021 article offered three recommended practices for handling sterile packaged medical products. You may be asking yourself: So, why revisit old news? The answer is simple. Looking back can offer an interesting perspective on what beliefs and strategies endure and when a flawed belief becomes a lesson learned instead.
As packaging professionals, this may seem a bit removed from our role. But what if the end-user experience with our customer’s product can be made safer, better, or more effective? Everyone in this industry holds patient safety and improving lives as top priorities. If our customers add value for their customers through packaging innovations, isn’t that good for everyone—including our own enterprises? With those questions in mind, we reviewed the three handling practices for sterile packaging through a different lens.

1. Proper Hand Hygiene
For all its seeming simplicity, consistently applied clinical hand-hygiene practices have remained a global challenge since emerging as a healthcare risk in the mid-19th century. It wasn’t until the U.S. Centers for Disease Control (CDC) issued guidelines in 1975 and again in 1985 that any formalization was proposed. The World Health Organization followed suit, issuing multiple iterations of guidelines on the topic beginning in the mid-1980s.
Hand hygiene compliance (HHC) progress and outcomes (though geographically varied) were not tracked until the early 2000s, at which point an American Journal of Infection Control paper found that 89.8 percent of healthcare workers in subject hospitals were aware of the guidelines, yet 44.2 percent of them had no program to improve HHC, with data hovering at about 50 percent compliance. Naturally, while not largely studied, this was not a stellar template for increasing hand hygiene practices in less advanced regions around the world.
If there was any silver lining from the global COVID-19 pandemic, it may have been that everyone on the planet, from clinician to child, became aware and more focused on hand hygiene protocols for safer, better health. A 2021 study from The Journal of the American Medical Association (JAMA) reported that the persistent “around 50%” U.S. facility HHC rates until the outbreak of COVID-19. In subsequently tracked U.S. hospitals, HHC rates shot up to 100 percent, based on data from March 28, 2020. Unfortunately, as the pandemic waned, so did HHC rates, landing back at the same pre-pandemic rates. Is there an opportunity here?
Medical device and pharmaceutical packaging considerations:
-
How can medical packaging professionals support and promote ongoing improvements in hand hygiene?
-
With more patient- and caregiver-administered medical care, are there packaging innovations that can protect sterility and use at home?
2. Storage and Transfer of Sterile Goods
Every clinic, office, surgical center, hospital, etc., has its own physical structure. Storage areas and containment are completely singular in multiple ways, and thus, not scalable. The original article suggested that receiving departments “properly clean” storage areas for sterile goods according to each State Health and Human Services Departments infection control regulations. A sound principle, yet also totally unique by facility, and dependent on a state’s regulatory climate.
Other storage and transfer suggestions included stocking product in such a way to ensure “first-in-first-out” rotation, avoiding moisture and transporting sterile products on “clean carts,” to store products without crowding or use of “binding” supplies (i.e., rubber bands) that could threaten packaging integrity. Common sense advice, to be sure, but perhaps impossible to meaningfully rein in for even local management.
Does the vastly heterogeneous nature of storing and transferring sterilely packaged medical products preclude adding value at the granular level through packaging features?
Medical device and pharmaceutical packaging considerations:
-
Could labeling or some other form of messaging to the receiver (both clinical and at-home) provide product-specific recommendations or concerns for in-house handling?
-
Are there product development opportunities where optimal “storage and transfer” accessories or aids could be marketed to support ideal handling?
-
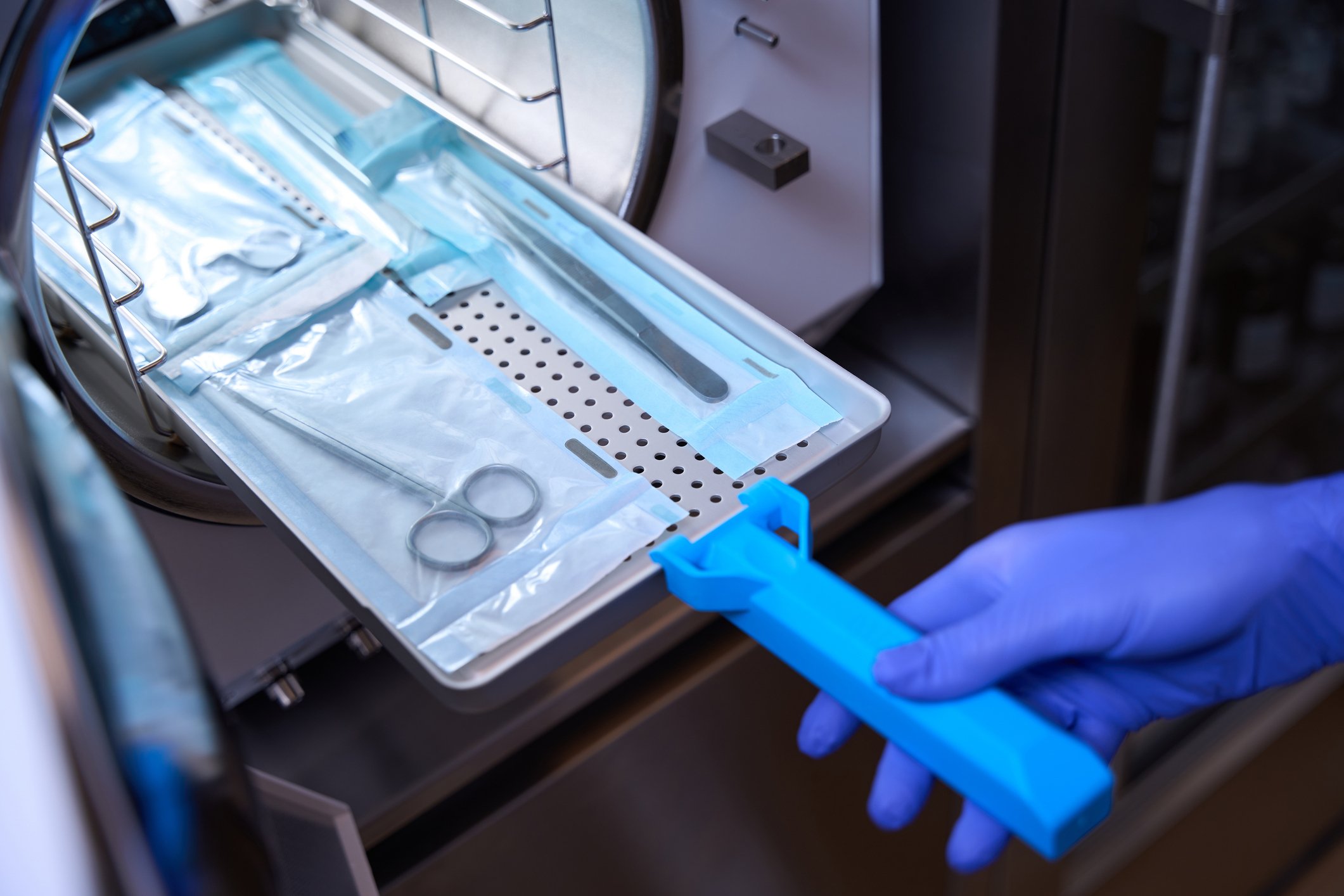
Handling and Opening of Sterile Goods
The final aspect presented in the original article is already familiar to the medical packaging industry. We have seen the rapid integration of human factors into packaging design and point of use, including the popularity of nurse panels to inform us as to what works and what doesn’t. The points made in the original article for this aspect of handling sterile goods reinforce the need for HHC at the time of opening and call out the need to repeat HHC at any potential point of contamination (i.e., touching your face). Inspection of the packaging and transport cart/tray disinfection were also identified. In short, we are actively innovating to accommodate the practical interface of humans with the medical product.
The likelihood of standardization is once again limited due to the non-scalable nature of product development and use, but certainly deserves to be a conversation topic as the details of a medical device or medicine are conceived. Are there opportunities for safety checks that could be part of packaging systems?
-
What about color-changing features or a ready-to-use sanitizing wipe or spray inside a kit as an extra measure over glove or hand?
-
Could color changing gloves reveal when someone has touched their face?
-
Does machine vision come into play?
You get the idea. There is always room for pioneering and that’s what makes healthcare packaging such a rewarding and creative field. Looking back helps us look forward. It also reminds us of human nature—and brings us back to the beginning, and perhaps the ultimate wildcard: how can we help the global healthcare community achieve and sustain optimal HHC (and more!)?